
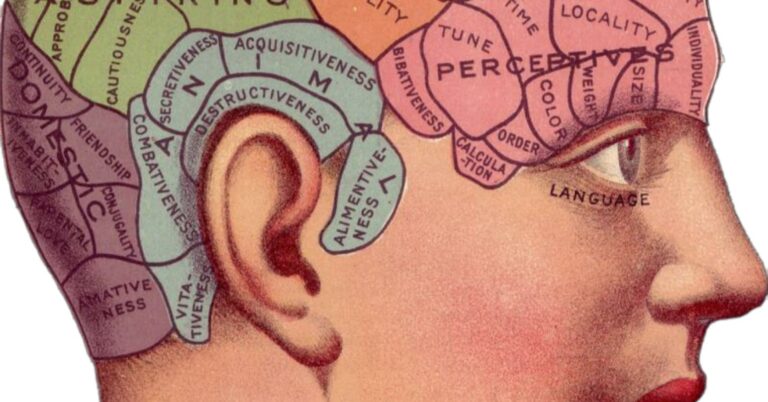
Source: AdinaVoicu / Pixabay
I avoid prescribing benzodiazepines and other addictive sedative-hypnotics whenever possible and caution students, readers, and colleagues to do the same. As an addiction psychiatrist, I generally feel that facing our pain, rather than numbing ourselves, is best for long-term mental health.
However, I recently read a darkly funny, thought-provoking, bestselling novel—My Year of Rest and Relaxation by Ottessa Moshfegh—that caused me to reflect on this issue in a slightly more nuanced way.
The Novel’s Plot (Spoiler Alert)
When the novel opens, we learn quickly that the protagonist (unnamed)—cynical, emotionally shut down, and self-absorbed—plans to spend as much time as possible sleeping throughout the next year by using pharmaceuticals. She claims it’s for self-preservation, and the reader is immediately skeptical.
We soon meet a hilarious hyperbole of a character, Dr. Tuttle, who is an unambiguously awful psychiatrist. She is easily manipulated, neglectful, and completely disconnected from her patients.
She pees loudly while on the phone with her patients. She prescribes increasingly strong sedatives for our protagonist in ridiculous combinations and warns of some absolutely horrifying-sounding side effects (e.g., “foaming at the mouth” and “perceived space-time anomalies”).
Their work together culminates in a prescription for a fictional medication, “Infermiterol,” to which the protagonist becomes physically tolerant (meaning the more she uses, the less and less it works). Dr. Tuttle (at this point, predictably) responds by raising the dose significantly instead of tapering.
Meanwhile, the protagonist spins out. As she anesthetizes herself more, she grows less and less generous. She is increasingly self-centered, unempathetic, and passive. She leaves her job early on and, in that way, no longer contributes much (at least, as far as society goes).
She is increasingly cold towards and disengaged from her friend Reva, who suffers through some major losses and other life stresses. At one point, the protagonist gives the frightening Infermiterol pill to Reva, and for a short while, we think she may have killed her. Sometimes, she’s downright mean to her friend.
The protagonist’s actions increasingly threaten her own well-being and safety, too. The drugs cause blackouts, and hers become more and more intense and prolonged. It is implied that our protagonist will go into life-threatening withdrawals if she runs out of medications. Towards the end, she chooses to make herself entirely vulnerable to an ethically questionable artist.
She locks herself in her apartment, gives him the only key, and allows him free to make art of her sleeping corpse while she checks out for months. Her judgment, we think, is undeniably impaired. Our worry for her livelihood grows with our empathy for her, too, as we learn more about her traumatic backstory.
By the end, we are certain she will end up killing herself or someone else, and no good will come of her situation. But Moshfegh subverts our expectations. The protagonist comes out of her deep sleep, healed. Her sleep did what she hoped. She has changed for the better.
Reborn, she now joyfully feeds birds cornflakes in the park, tells her friend Reva she loves her (saying what Reva always wanted to hear from her), and relinquishes the last of her material attachments, selling her deceased parents’ home.
In the final pages, she says,
I watched a bee circle the heads of a flock of passing teenagers. There was majesty and grace in the pace of the swaying branches of the willows. There was kindness. Pain is not the only touchstone for growth, I said to myself. My sleep had worked.
As summed up by Juliane Strätz in a compelling literary analysis:
She suddenly opens up to the world, is able to listen and affect the world, and is willing to be affected in turn. She has, in effect, relearned how to speak the affective language…She is receptive, attentive, open-minded, naïve, and most of all, alive. She has grown to experience the world in its entirety.
Better to Face Our Pain or Numb and Escape?
Reading this book reminded me that there are times when escape is what we need most, where looking away from our emotional pain or past trauma rather than straight into it is best. Moshfegh certainly highlights the pitfalls of both sides but, in the end, makes a good argument that sometimes escape is our best medicine.
Obviously, I’m not advocating we all go out and drug ourselves up with Infermiterol like Moshvegh’s extreme protagonist. But we should remember to give ourselves permission to turn away for a while when it’s needed—to numb—in a self-soothing way by engaging in behaviors that don’t heighten the risk of blackouts, tolerance, withdrawal, craving, and death. Some of my own personal (healthier) favorites include time in nature, exercise, socializing with friends or family, writing, learning, television and movies, doggie affection, and listening to Hip-Hop.
Better to Medicate Feelings Away or Confront Them, Like in Therapy?
As far as medicating goes, I stand firm on my position about benzodiazepines, which can cause tolerance, withdrawal, craving, and loss of control within a few weeks of initiating and can prevent evidence-based psychotherapeutic interventions from working, studies show. I still believe that benzodiazepines and related compounds should be used sparingly, if at all, despite this protagonist’s miraculous recovery. I suspect Moshfegh would probably agree. After all, it’s a work of fiction designed to make us think, not provide medical advice.
However, in terms of other pharmaceuticals though, many of our non-addictive psychiatric medications, such as SSRIs for depression or anxiety and anti-craving medications for addictions, can be life-saving, have few side effects and generally promote rather than detract from long-term mental health (when given to the right people at the right time).
Through dampening negative affect (anxiety, depression, craving), non-addictive psychotrotropics like SSRIs have the potential to help people engage and function better than ever. These medications can, when used appropriately, accelerate the progress of psychotherapy-based work or enhance self-reflection in the context of 12-step-based work, too.
Conclusion
So, which is better, escape or confrontation, medication or therapy? The answer: both. There are times for all of them.
In this novel, Moshfegh challenges us to consider prevailing beliefs that engagement, connection, and “going into the pain” are the only paths to psychological peace and raises some provocative questions. The truth is, checking out is sometimes the best medicine. We all need to get away and escape from the world and ourselves from time to time.
I invite you to consider some of the healthier ways you like to escape and in what settings it’s supportive, versus undermining, of your own long-term well-being.


















+ There are no comments
Add yours